Coronary artery disease (CAD) is now the most common type of heart disease and results in 370,000 deaths annually in the U.S.
Your Prescriptions Sorted and Delivered
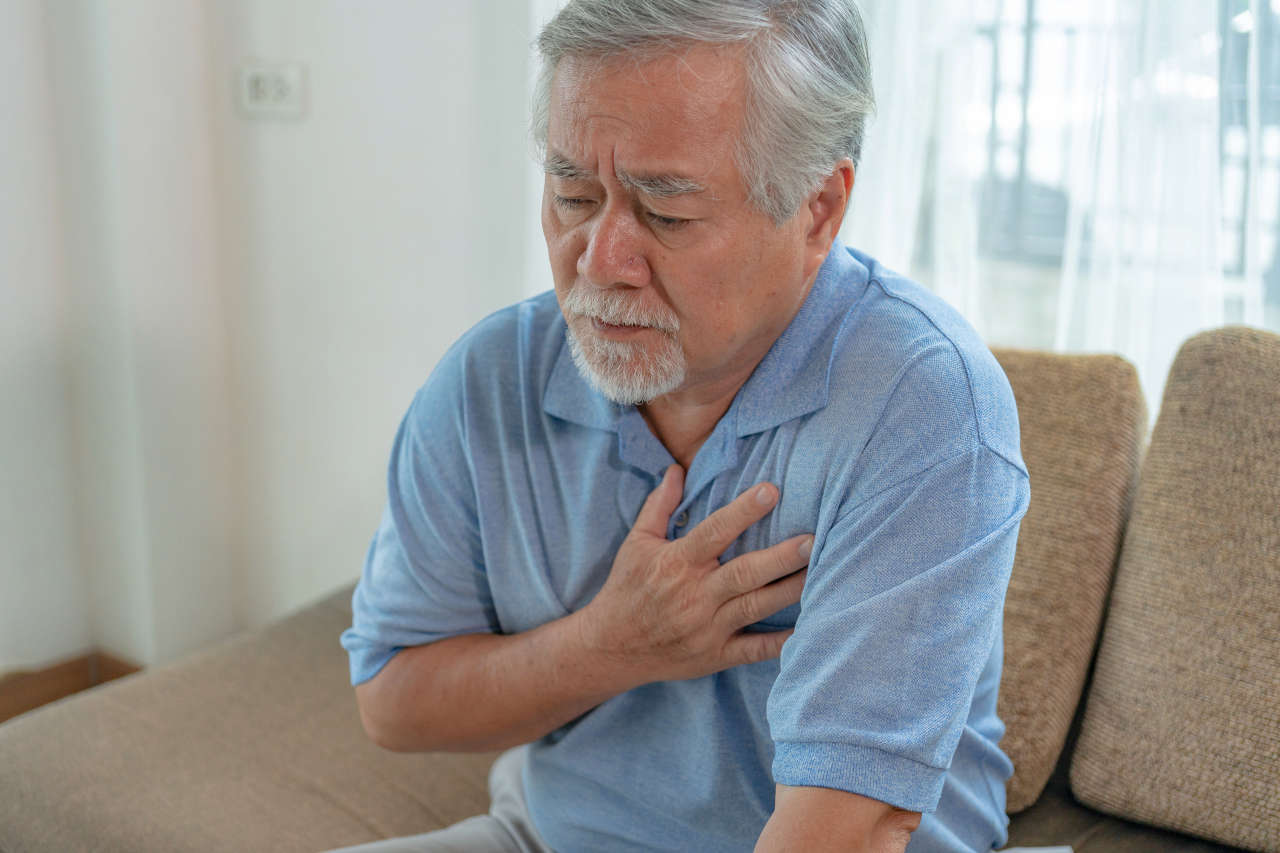
CAD can reduce blood supply to the heart muscle due to plaque buildup in the coronary arteries, causing symptoms like shortness of breath, chest pain, or rapid fatigue. If the narrowing of the arteries becomes severe, it may even cause a heart attack.
It is estimated that around 80 million women and 110 million men have coronary artery disease worldwide. So, what causes coronary artery disease, and how can we prevent it? Let’s discuss this in detail.
What Is Coronary Artery Disease?
Coronary artery disease (CAD) is the narrowing, hardening, or blockage of the coronary arteries, which supply oxygen-rich blood to the heart.
It occurs because cholesterol, fats, and other substances build up in the coronary arteries in the form of plaque (a sticky, waxy deposit), blocking blood flow to the heart. The building up of plaque in the coronary arteries is known as atherosclerosis.
Increased plaque in the coronary arteries can make them hard and narrow, reducing blood supply to the heart. A decreased blood and oxygen supply can cause weakness of the heart muscle, and a complete blockage in blood supply and oxygen can lead to a heart attack by permanently damaging the heart muscle.
Coronary Artery Disease Causes and Risk Factors
We know that coronary artery disease occurs due to plaque build-up in the coronary artery. An unhealthy lifestyle, diet, and certain medical conditions may contribute to plaque build-up, such as:
- Smoking
- Excessive alcohol consumption
- Low level of physical activity
- Obesity
- Stress
- A diet with high sodium or sugar
- Diabetes
- High cholesterol
- High blood pressure
- Chronic kidney disease or kidney failure
Other risk factors for coronary artery disease include:
- Male gender at birth
- Age over 35 years
- Family history of coronary artery disease
- Hispanic, Black, Southeast Asian, and/or Latino ethnicity
Symptoms of Coronary Artery Disease
The symptoms of coronary artery disease commonly start after a large amount of plaque has built up in the coronary arteries over many years. Common symptoms may include:
- Chest pain or heaviness
- Palpitations
- Fatigue
- Difficulty breathing or shortness of breath
- Dizziness or lightheadedness
- Cold sweats
- Heartburn
- Pain that spreads to the arms, shoulders, back, jaw, or neck
- Nausea
No More Pill Sorting! Our Pharmacy Pre-sorts and Packages Your Pills
Diagnosis of Coronary Artery Disease

A physical examination, blood tests, different types of X-rays, and cardiac procedures are used to diagnose coronary artery disease.
A healthcare provider first evaluates the blood pressure, medical history, diet, and lifestyle to determine the risk of heart disease.
Next, blood tests and cardiac procedures may be done to look for more evidence of coronary artery disease, like:
- Lipid profile blood test (for different fats)
- Electrocardiogram (ECG)
- Chest X-ray
- Exercise stress test
- Echocardiogram
- Computerized tomography (CT) of the coronary arteries for calcium or plaque
- Cardiac catheterization
Coronary Artery Disease Prevention and Treatment
Treatment recommendations for coronary artery disease will depend on how much it is affecting our daily function, what our symptoms are, how much the heart may already have been affected, and how severe it appears to be on testing. Options often include:
- Lifestyle changes for nearly everyone (exercise, diet, stress reduction)
- Medications to control symptoms, improve heart function, reduce risk factors, or prevent further damage
- Heart surgery or cardiac procedures to open the blood vessels
Studies show that cardiac rehabilitation programs with exercise, stress management, and nutritional guidance improve patient outcomes and reduce future cardiac events.
Lifestyle Changes
Lifestyle changes for treating and preventing coronary artery disease include eating a healthy, low-sodium and low-fat diet, exercising regularly (30 minutes for 5 days per week), reducing smoking as much as possible, and limiting alcohol consumption.
Other modifications include managing medical conditions that may contribute to coronary artery disease, like controlling blood sugar, cholesterol levels, and high blood pressure.
Persons with diabetes or high blood pressure should definitely monitor their blood sugar levels or blood pressure, and work on taking measures to improve them. Following a Mediterranean or DASH diet can be helpful in controlling both blood pressure and cholesterol levels.
Medications
Some of the common medications that help reduce plaque build-up in the arteries or manage blood pressure include:
Cholesterol-Lowering Medicines
Plaques are made of fatty substances and “bad” cholesterol (low-density lipoprotein, LDL).
Cholesterol-lowering medicines, like statins, fibrates, or niacin, help lower LDL cholesterol, reducing plaque in the coronary arteries.
Beta-Blockers
Beta-blockers are drugs that help lower blood pressure by blocking some of the effects of adrenaline, a hormone that increases heart rate and blood pressure.
Aspirin
Plaque formation in the coronary artery may increase the risk of blood clots. Aspirin is a drug that works as a blood thinner and may reduce the risk of clot formation.
Nitroglycerin
Nitroglycerin is a drug that relaxes blood vessels. It helps open up or widen the narrowed coronary artery, temporarily increasing blood flow to the heart.
Medbox: Never Sort Medications Again
Heart Surgery or Cardiac Procedures
The following surgeries or procedures are used to improve blood flow or remove plaque buildup in a blocked coronary artery:
Coronary Artery Bypass Graft Surgery
A coronary artery bypass surgery is a procedure in which the surgeon takes an artery or vein from another part of the body and uses it to create a new pathway around the blockage in a coronary artery, through which blood can flow to the heart muscle.
Stent Placement
A stent is a small mesh tube that can be placed inside a coronary artery to keep the narrowed or blocked artery open, allowing blood to flow to the heart muscle.
This is done during a cardiac catheterization, which is a procedure performed by threading a very long, thin tube called a catheter through a large blood vessel of the body all the way up to the heart. It is then passed into the coronary arteries to allow the cardiologist to see blockages and try to repair them.
Coronary Angioplasty
In this procedure, a catheter with an attached inflatable balloon is inserted into a blocked coronary artery. The balloon is inflated to open up the clogged coronary artery and improve blood flow.
The best treatment of all for coronary artery disease is, of course, preventing it from starting or getting worse. A common saying about our life circumstances says that we are one-third what we are born with, one-third what happens to us, and one-third what we do with it. While we cannot change our native risk factors and often cannot change what happens to us, we can certainly change what we do with what we are given. We can start to work on our strategies for prevention of disease today.
REFERENCES:
- National Center for Health Statistics. Multiple Cause of Death 2018–2022 on CDC WONDER Database. Accessed July 24, 2024. https://wonder.cdc.gov/mcd.html